






InUrSkn is more than just a skin a hair and body clinic. It is Dr. Sejal's promise of providing minimal intervention patient care which is holistic, personalized and humane.












Psoriasis is a chronic, cyclical disorder characterized by red, itchy lesions with silvery flakes caused by rapid skin cell growth. It often affects the nails as well. The condition may go into remission for periods but tends to recur, commonly appearing on the lower back, elbows, knees, and scalp. Approximately 25% of cases also involve psoriatic arthritis.
Triggers include factors such as stress and weather changes, while the underlying cause is linked to immune system dysfunction. Management typically involves oral or topical medications and light therapies, such as the Excimer Laser, aimed at controlling flare-ups and relieving symptoms.
Read More
Vitiligo is an autoimmune disorder in which the immune system attacks the skin’s melanocytes, leading to the development of white patches. Onset typically occurs between the ages of 30 and 50, with progression that can be unpredictable. Common triggers include stress and skin trauma. Treatment options vary depending on the severity of the condition.
Read More
Eczema, or atopic dermatitis in children, is a chronic but manageable skin condition characterized by itchy, red rashes, often accompanied by oozing fluid and dry, cracked skin. Genetic variations can affect the skin’s ability to retain moisture. Management typically includes regular moisturizing, avoiding irritants, using prescribed medications, and making lifestyle adjustments.
Read More
Rosacea, often recognized by flushed red cheeks, presents as painful bumps or boils on the face—mainly on the cheeks or nose—along with frequent flushing. While the exact cause remains unknown, it is believed to result from a combination of hereditary, environmental, and immune system factors. Often misdiagnosed as other skin conditions like acne, rosacea may also be accompanied by eye symptoms such as watering or burning. Common triggers include hot drinks, spicy foods, and emotional stress. Treatment primarily involves topical and oral medications to regulate blood flow and reduce bumps, helping manage the symptoms effectively.
Read More
Lichen Planus is a chronic autoimmune condition that affects the skin, mucous membranes, hair, and nails—most commonly in middle-aged adults. It typically causes small, flat, purplish lesions. Management involves medications to control symptoms and prevent complications.
Read More
Hives, or urticaria, are caused by allergic reactions and appear as itchy, raised bumps with a red or pink hue. Common triggers include certain foods, insect bites, medications, or sun exposure. Chronic hives may indicate an underlying condition and are typically managed with antihistamines or moisturizing emollients.
Read More
Lupus is an autoimmune disease in which the immune system mistakenly attacks the body’s own tissues and organs. It can affect multiple body systems, including the skin, hair, kidneys, joints, and heart, and is most common in females aged 20 to 40. The condition manifests in three main types—acute, subacute, and chronic lupus—with symptoms such as skin lesions, hair loss, and joint pain. Triggers include sunlight, certain medications, and infections. Diagnosis typically involves specific blood tests and imaging studies, while treatment includes oral medications and sun protection.
Read More
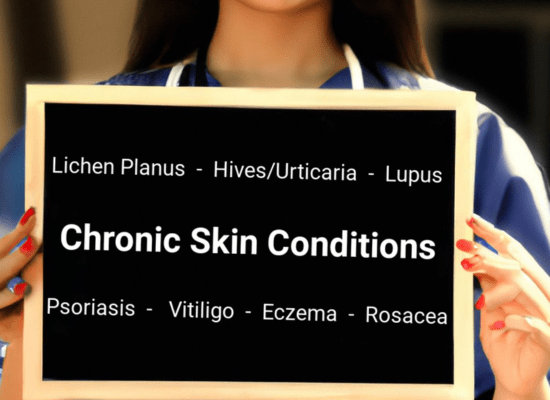
Chronic skin conditions are persistent ailments that affect the integumentary system (skin, hair, nails, and mucous membranes), often lasting for many years or even a lifetime. Unlike acute conditions, which may resolve with time or treatment, chronic skin issues typically require ongoing management to control symptoms, minimize flare-ups, and maintain an individual’s quality of life. Common chronic skin conditions include eczema, psoriasis, rosacea, vitiligo, lichen planus, and chronic hives (urticaria).
These conditions may present a range of symptoms such as inflammation, itching, redness, scaling, pigmentation changes, and, in some cases, pain. The exact cause of many chronic skin conditions remains unclear, but they often involve genetic, immunological, and environmental factors. Additionally, they may be associated with other systemic conditions or have comorbidities—such as psoriatic arthritis in the case of psoriasis, or eye complications in the case of rosacea.
Management may involve topical and oral medications, light therapy, lifestyle modifications, and, occasionally, surgical interventions. While these conditions are typically not curable, appropriate medical care and lifestyle changes can significantly alleviate symptoms and improve the skin’s appearance. It is crucial for individuals with chronic skin conditions to work closely with dermatologists to develop a personalized management plan that meets their specific needs and enhances their overall well-being.

Dr. Sejal understands that treating a chronic condition is not just about reducing symptoms, but about improving the patient’s overall quality of life. Many chronic skin conditions can lead to social anxiety and often require cosmetic solutions as well. Dr. Sejal brings over 15 years of experience in both dermatology and cosmetology to the treatment and care of such conditions. She offers a holistic approach to managing chronic skin issues, which includes the following:
Detailed Assessment and Diagnosis
Patient Education
Personalized Treatment Plans
Lifestyle Recommendations
Long-term Monitoring and Follow-up
Emotional and Psychological Support
Coordination with Other Healthcare Professionals
Encouragement of Patient Self-management

Psoriasis is a chronic (long-lasting) condition that can be controlled but not cured. It presents as multiple itchy red lesions with silvery white flakes. This formation of skin flakes occurs due to the rapid growth of skin cells. Nails are often also affected.
Psoriasis is a cyclical disorder in which the condition may flare up for a few weeks or months and then go into remission—only to return again.
It is commonly seen on the lower back, elbows, knees, palms, soles, scalp, etc. It can be localized or generalized.
In about 25% of cases, it is accompanied by psoriatic arthritis.
Common symptoms of psoriasis include:
Red patches of skin covered with thick, silvery scales
Small scaling spots
Dry, cracked skin that may bleed or itch
Itching, burning, or soreness
Thickened, pitted, or ridged nails
Swollen and stiff joints
Psoriasis is caused by a malfunction of the immune system. The exact reason for this malfunction remains unknown.
People at a higher risk of developing psoriasis include those with:
Psoriasis may be aggravated by the following factors:
Psoriasis lesions are treated with a combination of oral and topical medications. Additionally, they may be treated using light therapy. At InUrSKn, we offer the following light-based treatment for psoriasis:
Excimer Laser
Common triggers include stress, certain medications, skin injuries, infections, and weather changes.
Some individuals find relief by reducing alcohol, gluten, or nightshades, though results vary.
Yes, types include Plaque, Guttate, Inverse, Pustular, and Erythrodermic psoriasis.
No, psoriasis is not contagious and cannot spread between individuals.
No, it can also affect nails and joints, a condition known as psoriatic arthritis.
Sunlight can be beneficial in moderation, but sunburn can trigger flare-ups.
Yes, it can be associated with heart disease, diabetes, and other auto-immune disorders.
Stress can trigger flare-ups and managing stress can potentially reduce symptoms.
There’s no cure, but treatments can manage symptoms and improve quality of life.
They have different appearances, and a dermatologist can provide an accurate diagnosis.

Vitiligo is an autoimmune condition in which the body’s immune system attacks melanocytes—cells responsible for producing melanin, the pigment that gives our skin its color. When melanocytes are destroyed, melanin production stops in the affected areas, causing the skin to turn white.
Vitiligo is not a contagious disease. It can develop at any age but is most commonly seen between 30 and 50 years. It typically appears as well-defined white or discolored patches on the skin, often affecting the hands, legs, and face.
Hair in the affected areas may also turn white.
Unfortunately, the progression of vitiligo is unpredictable—it can worsen or improve rapidly over time.
While the exact cause is unknown, vitiligo is known to have a hereditary link. As an autoimmune disorder, it results from the immune system malfunctioning and attacking healthy cells.
Common triggers include:
Vitiligo is also often associated with other autoimmune conditions like diabetes and thyroid disorders.
As there are no clearly known causes besides hereditary factors, prevention is limited. However, one of the most effective strategies recommended by Dr. Sejal is stress management. Techniques such as regular exercise, meditation, or even simple relaxation activities like watching television can help reduce stress and possibly minimize flare-ups.
Dietary habits and environmental exposures have shown weak associations with vitiligo, so managing these aspects is unlikely to significantly affect its progression.
Vitiligo treatment generally follows one of the following approaches:
Camouflage
Suitable for mild, localized cases. Small depigmented patches on visible parts of the body are concealed with temporary or semi-permanent makeup. Treatments like microblading can provide longer-lasting coverage by blending pigments with surrounding skin tones.
Regaining Natural Melanin
Also ideal for mild, localized vitiligo. Therapies like excimer lasers and other UV-based treatments stimulate melanin production in affected areas, helping restore pigmentation.
Depigmentation of Remaining Skin
For widespread or severe vitiligo, depigmentation may be considered. In this approach, pigmented areas are treated with topical agents to lighten the skin, creating a uniform appearance. This is a serious decision and must be guided carefully by a qualified dermatologist.
No, vitiligo is not contagious and there’s no need to avoid contact with affected individuals.
Yes, vitiligo affects individuals of all ethnicities and races. It may be more noticeable on darker skin, but it occurs equally.
No, vitiligo is an auto-immune condition unrelated to dietary or lifestyle choices.
No, untreated vitiligo may progress. It’s advisable to consult a dermatologist for treatment options as soon as it’s diagnosed.
Yes, treatments like topical and oral medications, as well as light therapies that stimulate melanin production, can help manage vitiligo.
Sun exposure does not typically affect vitiligo, but protecting the skin from sunburn and excessive sun exposure is advisable. Other environmental conditions generally do not affect vitiligo.
No, vitiligo and skin cancer are unrelated conditions, although individuals with vitiligo can develop skin cancer like anyone else.
No known natural or herbal remedies have been proven effective for vitiligo. It’s advisable to consult a dermatologist for treatment.

Eczema is a chronic (long-lasting) condition that is controllable but unfortunately not curable. It presents as itchy, red rashes that may ooze fluid and are often accompanied by cracked and dry skin. It can occur at any age. When it occurs in children, it is referred to as atopic dermatitis. Eczema can appear on any part of the body and is not contagious.
Symptoms of eczema include:
Eczema commonly appears on areas such as the hands, feet, ankles, wrists, neck, upper chest, eyelids, and inside the bends of the elbows and knees. In infants, it may also affect the face and scalp.
Eczema is primarily genetic in nature, meaning that a variation in a gene causes the skin to lose its ability to retain moisture, leading it to dry out quickly. This, in turn, makes the skin more susceptible to allergens, irritants, and environmental factors.
Prevention and control of eczema flare-ups can be achieved by:
Eczema is largely treated with a combination of oral and topical medications, along with appropriate lifestyle and habit changes.
Yes, certain food allergies can trigger eczema flare-ups, particularly in children. Common triggers include eggs, dairy, nuts, and soy.
Yes, dry or cold climates can worsen eczema symptoms as they can dry out the skin further. Humid climates may provide some relief.
Yes, stress is known to trigger or worsen eczema flare-ups in some individuals.
Yes, eczema is often associated with other allergic conditions like asthma and hay fever.
Eczema doesn’t spread like an infection, but it can appear on different parts of the body at different times.
Currently, there’s no permanent cure for eczema, but treatments can effectively manage and alleviate symptoms.
It’s recommended to moisturize the skin at least twice a day, or more often if necessary to keep the skin hydrated.
Over-the-counter creams may help with mild eczema, but it’s advisable to consult with a dermatologist for persistent or severe cases.
Yes, scratching can worsen eczema and potentially cause infection if the skin is broken.
Some individuals find relief by eliminating foods that trigger allergies, though it’s advisable to consult with a healthcare provider before making significant dietary changes.

Flushed red cheeks may be a sign of Rosacea, a condition that differs from naturally healthy red cheeks. It typically presents as red, painful bumps or boils on the cheeks or nose and is often accompanied by facial flushing. In some cases, symptoms may also include eye-related issues such as watering or a burning sensation.
Rosacea is often mistakenly diagnosed as other skin conditions like acne.
The exact cause of rosacea is unknown, but it is believed to result from a combination of hereditary, environmental, and immune system-related factors.
People more likely to develop rosacea generally fall into the following demographics:
Rosacea can be triggered or aggravated by the following factors:
Avoiding these triggers can help reduce the frequency and severity of rosacea flare-ups.
Rosacea is primarily treated using topical and oral medications that regulate blood flow and reduce bumps and pimples.
No, there isn’t a cure for rosacea, but with proper treatment and management, its symptoms can be controlled.
No, rosacea is not a contagious condition.
Yes, in severe cases, rosacea can cause skin to thicken, especially around the nose.
Yes, ocular rosacea can cause redness, irritation, and swollen eyelids.
Laser treatment can be effective in reducing redness and visible blood vessels associated with rosacea.
Yes, sun exposure can trigger or worsen rosacea flare-ups. Wearing sunscreen and protective clothing is advisable.
Some studies suggest a connection between gastrointestinal disorders like SIBO and rosacea. Further consultation with a healthcare provider is advisable.
Individuals with rosacea should avoid harsh or abrasive skincare products, as well as those containing alcohol, witch hazel, or fragrances.
Rosacea can worsen over time without treatment, though individuals may experience periods of remission.
Over time, untreated rosacea can lead to permanent changes such as skin thickening or visible blood vessels.

Lichen Planus is a chronic condition affecting the skin, mucous membranes, hair follicles, and nails. It can occur at any age but is more commonly seen in middle-aged adults.
It presents as small, flat-topped, purplish lesions typically found on the wrists, legs, back, backs of the hands, and sometimes the genitals. Inside the mouth, it appears as whitish lesions and ulcers. Thicker lesions may also be seen on the palms and soles.
The nails may develop thick ridges and show signs of damage or destruction. Hair loss can also occur and may be either scarring or non-scarring in nature.
Lichen Planus is an autoimmune condition, wherein the body’s immune system mistakenly attacks healthy cells in the skin and mucosa.
It is most commonly seen in middle-aged individuals. Possible contributing factors include:
Certain medications and vaccines—such as painkillers and arthritis medications—are known to trigger Lichen Planus. Additionally, some dental treatments involving mercury may also act as triggers.
Stress is another factor that can contribute to flare-ups.
Potential complications of Lichen Planus:
Treatment options include:
No, Lichen Planus is not contagious and cannot be spread from person to person.
Yes, although it’s more common in middle-aged adults, it can occur in children.
There is no cure for Lichen Planus, but treatments can help manage symptoms and alleviate discomfort.
Yes, the lesions from Lichen Planus can heal and leave behind long-lasting marks or scars.
Yes, certain medications, stress, and exposure to allergens and irritants can trigger flare-ups.
Yes, it can affect the skin, mucous membranes, nails, and hair follicles.
Lichen Planus has been associated with Hepatitis C infection in some cases.
Yes, it can sometimes be mistaken for other skin conditions, making correct diagnosis is crucial for appropriate treatment.
Treatments may include topical corticosteroids, antihistamines, immune modulators, and retinoids, depending on the severity of the condition.
Yes, Lichen Planus can recur, and it may come and go over many years.

Hives are nothing but an allergic reaction that presents as itchy, raised bumps. These bumps can occur on any part of the body. They are usually red, pink, or flesh-colored, and sometimes they may sting or hurt.
Allergic reactions occur when the body releases histamines into the bloodstream. Histamines are chemicals produced by the body to defend itself against infections and foreign substances. In some individuals, these histamines can cause swelling, itching, and other symptoms.
Most people experience hives as a temporary condition, in which case the lesions go away on their own or with the use of anti-allergy medication. However, in some cases, hives can become a chronic condition accompanied by other health issues.
The different reasons for allergic reactions that may lead to hives include:
Unfortunately, in most cases, it is not possible to identify the exact cause.
If you suffer from chronic hives, you may have an underlying condition such as:
Since hives are an allergic reaction, they can only be prevented by avoiding exposure to the triggering factor. However, it is often very difficult to determine the exact cause. Symptomatic treatment for hives typically includes the use of antihistamines. For immediate relief, a doctor may also prescribe a moisturizing emollient.
The common symptoms include itchy, red or flesh-colored bumps or welts on the skin, which may sting or hurt.
Acute hives may last less than six weeks, while chronic hives can last more than six weeks, sometimes even years.
No, hives are not contagious and cannot spread from person to person.
There is no cure for chronic hives, but symptoms can be managed with medications and lifestyle adjustments.
Hives are diagnosed based on a physical examination and your medical history. Further tests might be necessary if chronic hives are suspected.
Antihistamines are the most common medication used to treat hives, and in severe cases, corticosteroids or epinephrine might be used.
Yes, stress can be a trigger for hives in some individuals.
It’s advisable to see a doctor if hives persist, are severe, or if you experience other symptoms like difficulty breathing.
Yes, chronic hives can sometimes be a sign of underlying conditions such as auto-immune diseases.
Cool compresses or baths, wearing loose-fitting clothes, and avoiding irritants can help alleviate symptoms, but it’s important to consult with a healthcare professional for persistent or severe cases.

Lupus is an autoimmune condition where the body’s immune system attacks its own tissues and organs. It can affect multiple systems in the body, causing inflammation of the skin, hair, kidneys, joints, blood vessels, brain, and heart. Lupus most commonly occurs in females between the ages of 20 and 40.
Lupus can present in three main types:
Subacute and chronic forms are usually limited to skin involvement.
Lupus is an autoimmune condition influenced by the following:
Triggering factors:
Diagnosis may include a thorough examination by a healthcare provider, discussing symptoms and medical history, along with specific blood tests, like Antinuclear Antibody (ANA) test, and imaging tests.
Yes, besides Cutaneous Lupus, there is Systemic Lupus Erythematosus (SLE), which is more severe and affects many organs, and Drug-induced Lupus, triggered by certain medications.
No, lupus is not considered rare, although its prevalence can vary among different populations and regions.
It can be, especially if major organs are affected or complications arise. However, with proper management, many individuals with lupus can maintain a good quality of life.
Yes, complications may include kidney damage, heart and lung issues, or neurological problems, among others, which can significantly impact a person’s health.
Currently, there is no cure for lupus, but its symptoms and complications can often be managed with medical treatment and lifestyle adjustments.
Besides medical treatment, maintaining a balanced diet, avoiding sun exposure, managing stress, exercising regularly, and avoiding known triggers can help manage symptoms.
Although the exact cause is unclear, individuals with a family history of lupus or other auto-immune diseases may be at a higher risk.
Yes, lupus can cause complications in pregnancy. It’s essential for women with lupus to consult with healthcare providers when planning for pregnancy.
Generally, yes, but it’s essential to consult with healthcare providers to determine which vaccinations are safe and recommended.


MD, DNB - Dermatology & Venereology
Dr. Sejal has dual degrees of MD and DNB in Dermatology and Venereology. She has worked with some of the senior most doctors in the largest government and private hospitals for more than 15 years. Over these years at InUrSKn, she has treated thousands of patients for a variety of conditions and needs across dermatology, venereology, cosmetology and trichology domains.
Dr. Sejal believes in a minimum intervention approach to health and believes that educating and empowering the patient is the key to good health.
Every patient at InUrSkn is seen personally by Dr. Sejal without any time limit, where she discusses the patient’s concern in detail along with understanding the history of their health and carrying out a personal examination.

At InUrSkn we belive that all patient care must be
– Holistic
– Personalized
– Humane
– Minimal
That is Dr. Sejal and Team live by the philospohy to never prescribe medications or procedures that may not be required and while approaching a concern Dr. Sejal ensures that a detailed history and context is understood by her. Medical tests are prescribed by Dr. Sejal when she believes that there is more to the concern which needs to be addressed and only then the patient can truly benefit.
Multiple spacious procedure rooms
Full-fledged operation theatre
In-house laboratory
Latest technology
100+ Skin, Hair & Body Procedures offered
Frequent disinfection of all clinic spaces with UVC light and WHO-approved chemicals
Large waiting and treatment areas to ensure social distancing
Regular health checks for all patients and staff
Safer than salons, chain-clinics & hospitals
PPEs for patients and staff
Personal attention from Dr. Sejal Saheta (MD, DNB) - with 15+ years of experience
CIDESCO-certified aestheticians with minimum 3 years work experience
500+ Positive Reviews on Practo and Google
5000+ Patients treated last year alone
8000+ Procedures completed
| Prices | ||
|---|---|---|
| Procedure | ||
| In Clinic Consultation with Dr. Sejal | ||
| In Clinic Consultation with Dr. Sejal | ₹1200 | |
| Online Consultation with Dr. Sejal | ||
| Online Consultation with Dr. Sejal | ₹1000 | |
Pricing (Inclusive of taxes)


Triggers can vary widely among different chronic skin conditions and individuals, common ones include stress, allergens, irritants, infections, hormonal changes, and genetic factors.
Most chronic skin conditions are not curable but can be managed effectively with the right treatment plan to control symptoms and prevent flare-ups.
Certain foods may trigger or worsen symptoms in some individuals. A dermatologist might suggest an elimination diet to identify potential food triggers.
Dermatologists are the primary specialists for treating chronic skin conditions, though in cases of associated comorbidities, other specialists might be involved.
Stress can exacerbate symptoms of chronic skin conditions as it may trigger an immune system response that worsens inflammation.
Typically, chronic skin conditions like eczema, psoriasis, or rosacea are not contagious, but it’s always best to consult with a healthcare provider for accurate information.
Treatments may include topical creams, oral medications, light therapy, immunosuppressive drugs, lifestyle modifications, and sometimes surgical interventions.
Over-the-counter creams, prescription ointments, and avoiding known irritants can help manage itchiness. It’s important to consult with a healthcare provider for personalized advice.
Prevalence and severity of chronic skin conditions can vary across different age groups and genders, often influenced by genetic, hormonal, and environmental factors.
Yes, weather changes can affect chronic skin conditions. Cold, dry weather may worsen symptoms, while warmer, humid climates might offer relief for some individuals.
Yes, discomfort and itchiness from chronic skin conditions can interfere with sleep, and poor sleep may, in turn, worsen skin symptoms.
Smoking and alcohol can worsen symptoms of many chronic skin conditions due to their effects on the immune system and blood vessels.
Regular monitoring and follow-up appointments with healthcare providers can ensure that the treatment plan remains effective and adjusts to any changes in the condition.
Yes, dealing with persistent symptoms and physical discomfort can lead to anxiety, depression, or self-esteem issues, emphasizing the importance of psychological support in management plans.
Effectiveness can vary greatly among individuals. It’s important to discuss any alternative treatments with a healthcare provider to ensure they won’t interfere with existing treatment plans or worsen the condition.


Ready to book an appointment?
BOOK

Want to talk about your needs ?
MAKE AN enquiry
