






InUrSkn is more than just a skin a hair and body clinic. It is Dr. Sejal's promise of providing minimal intervention patient care which is holistic, personalized and humane.













Human Papillomavirus (HPV) is a common viral infection transmitted through skin-to-skin contact and includes over 100 variants. More than 40 of these types, spread primarily through sexual contact, can affect the genitals, mouth, or throat. While many HPV infections remain asymptomatic, some may lead to genital warts or even cancers of the cervix, anus, or throat. Transmission does not require intercourse, making it relatively easy to contract. Preventive measures include practicing safe sex, using condoms, and getting vaccinated. Although the infection often resolves on its own, genital warts caused by HPV can be treated with procedures such as cauterization.
Read More
Chlamydia, a common sexually transmitted disease (STD), is caused by a bacterial infection and is often asymptomatic in its early stages. When symptoms do occur, they may include pain, a burning sensation during urination, and abnormal genital discharge. Prevention primarily involves practicing safe sex and using condoms. As a bacterial infection, Chlamydia is easily treatable with topical or oral antibiotics, offering a straightforward path to recovery with appropriate medical care.
Read More
Genital herpes, a common STD, is caused by the herpes simplex virus and typically presents as painful blisters in sensitive areas, often accompanied by fever. The virus enters the body through skin abrasions or mucous membranes and integrates into cells, making treatment difficult. Symptoms include blisters, itching, and, in some cases, swollen lymph glands. Prevention involves consistent condom use and safe sex practices. While antiviral drugs can speed up recovery, they do not eliminate the virus, leaving a possibility of recurrence—especially during periods of low immunity.
Read More
Syphilis, a bacterial STD, initially appears as a small, painless sore called a chancre, which can develop on the genitals, rectum, or inside the mouth. It is transmitted only through direct contact with these syphilitic sores. If left untreated, the infection can progress and cause severe damage to vital organs such as the heart and brain. As it advances through different stages, symptoms may include skin rashes, sore throat, and, in severe untreated cases, life-threatening tertiary syphilis. Preventive measures include using condoms and practicing safe sex. Syphilis can be effectively treated with antibiotics, especially when diagnosed in the early stages.
Read More
Crabs, or pubic lice, are tiny insects that reside in the pubic hair around the genitals, but they can also infest other hairy areas of the body such as the armpits, chest, and even eyebrows. Transmission primarily occurs through close physical contact, especially during sexual activity, although sharing clothing, linens, or towels with an infested person can also spread the lice. Despite the name, casual contact typically does not lead to transmission. These parasites can be effectively eradicated using specific medications, such as shampoos and creams designed to kill lice.
Read More

Venereal diseases, commonly referred to as sexually transmitted diseases (STDs) or sexually transmitted infections (STIs), are illnesses transmitted through sexual contact. They are caused by a variety of organisms, including bacteria, viruses, and parasites. Transmission occurs when individuals engage in vaginal, anal, or oral sex without adequate protection, such as condoms. Some well-known venereal diseases include chlamydia, gonorrhea, syphilis, herpes simplex virus (HSV), human papillomavirus (HPV), and HIV/AIDS, among others.
The symptoms of these infections can vary widely, ranging from no symptoms at all to severe discomfort or long-term health issues. For instance, untreated chlamydia or gonorrhea can lead to pelvic inflammatory disease in women, potentially resulting in infertility. Additionally, certain types of HPV can cause genital warts and cancers of the cervix, anus, and throat.
Prevention of venereal diseases primarily depends on practicing safe sex, which includes using condoms correctly and consistently, limiting the number of sexual partners, and getting tested for STDs regularly. Vaccines are also available for some STDs, such as HPV and hepatitis B, and provide effective protection.
Early diagnosis and treatment are crucial for managing venereal diseases and preventing complications. Treatment may include antibiotics for bacterial infections, antiviral drugs for viral infections, and other appropriate medical interventions, depending on the specific disease. Through education, vaccination, and responsible sexual behavior, the spread of venereal diseases can be significantly reduced.

Dr. Sejal strongly believes that for society to truly evolve, we must remove the stigma associated with STDs and focus our energy on educating the youth and making medical care more accessible to those affected by these conditions.
Dr. Sejal understands that it is not enough to simply treat STDs; there is also a critical need to counsel patients who are dealing with such conditions. Her approachable personality ensures that patients feel comfortable and free to express their concerns, allowing them to truly benefit from a consultation with her.
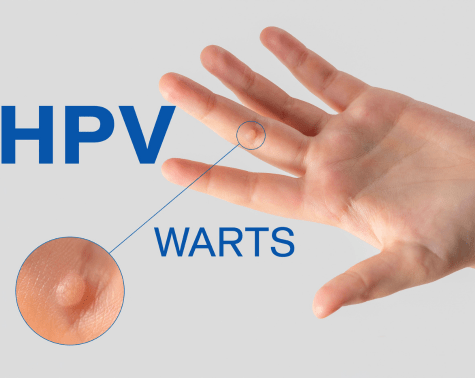
Human papillomavirus (HPV) is a viral infection transmitted through skin-to-skin contact. There are over 100 types of HPV, with more than 40 strains spread through sexual contact that can affect the genitals, mouth, or throat.
In many cases, genital HPV infections do not cause any health problems. However, certain types of HPV can lead to the development of genital warts and even cancers of the cervix, anus, or throat.
The virus that causes HPV infection is transmitted through skin-to-skin contact. Most people contract genital HPV through direct sexual contact, including vaginal, anal, and oral sex.
Since HPV is a skin-to-skin infection, intercourse is not required for transmission to occur.
Many people have HPV without knowing it, which means you can still contract it even if your partner shows no symptoms. It is also possible to be infected with multiple types of HPV.
The easiest ways to prevent HPV are by using condoms and practicing safe sex.
In addition, a vaccine is available to prevent genital warts and cancers caused by HPV. It protects against nine types of HPV known to be associated with either cancer or genital warts.
Most forms of HPV resolve on their own. In the case of genital warts, they can be treated through a simple dermatological procedure called cauterization, using one of the following techniques:
CO₂ Laser Excision
RF Cauterization
Scalpel Excision
Cryotherapy
Early symptoms may include genital warts, though many types of HPV do not cause any noticeable symptoms.
A healthcare provider can perform a Pap test for women to detect cervical changes, or an HPV DNA test. Men can have a visual inspection for warts, though there isn’t a definitive test for men.
There’s no cure for HPV, but the body’s immune system often clears the virus on its own. Treatments are available for the symptoms and complications like warts and cancers caused by HPV.
Yes, both men and women can receive the HPV vaccine to protect against some common types of the virus.
The HPV vaccine is recommended for all boys and girls starting at ages 11 or 12, though it can be given as early as age 9, and up through age 26 for those who did not get vaccinated earlier.
It’s generally not recommended for pregnant women to receive the HPV vaccine, but they should discuss this with their healthcare provider.
Generally, HPV doesn’t affect fertility, but some complications arising from certain high-risk types of HPV may potentially affect fertility.
The frequency of screening depends on age and previous test results. Women should follow the screening guidelines provided by their healthcare provider, usually starting from age 21.
While most HPV transmissions occur through sexual contact, some types can be transmitted through non-sexual skin-to-skin contact.
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking can help boost your immune system to clear HPV and reduce its symptoms.
Chlamydia is a common sexually transmitted disease (STD) caused by bacteria. Many people with chlamydia do not show any symptoms initially. In some cases, it may cause symptoms such as pain, a burning sensation during urination, and abnormal discharge from the penis or vagina.
Like all STDs, the best way to prevent chlamydia is by using condoms and practicing safe sex.
Since chlamydia is a bacterial infection, it can be effectively treated with both topical and oral antibiotics.
Chlamydia can be diagnosed through urine tests or swab tests conducted by a healthcare provider.
No, chlamydia requires treatment with antibiotics to be cured. Without treatment, it can lead to serious health problems.
Yes, if left untreated, chlamydia can lead to pelvic inflammatory disease in women and epididymitis in men, which can cause infertility.
It’s advisable to wait 1-2 weeks post exposure before getting tested to ensure accurate results. However, one should consult with a healthcare provider.
Typically, it takes about 7-14 days of antibiotic treatment to cure chlamydia, though one might be advised to abstain from sex for a week after starting therapy.
Yes, previous infection does not provide immunity, and you can get re-infected if exposed again.
Yes, STD treatment including chlamydia is confidential, but it’s important to inform sexual partners so they can also get tested and treated if necessary.
Untreated chlamydia can cause serious and permanent health problems like pelvic inflammatory disease, infertility, and ectopic pregnancy.
Yes, chlamydia can cause complications like premature birth, low birth weight, and infections in the newborn. It’s important to get tested and treated.
If treated timely, chlamydia shouldn’t cause any long-term effects. Untreated chlamydia can lead to serious health issues like infertility.
Genital herpes is a very common sexually transmitted disease (STD). It presents as painful blisters on sensitive areas, often accompanied by fever and a burning sensation at the affected sites.
The virus enters the body through skin abrasions or mucous membranes. Mucous membranes are thin layers of tissue that line the openings of the body, such as the nose, mouth, and genitals. Once inside, the virus integrates into your cells. Viruses tend to multiply and adapt to their environment easily, which makes them difficult to treat.
Two types of the herpes simplex virus (HSV) cause genital herpes:
HSV-1: This type usually causes cold sores but can also cause genital herpes.
HSV-2: This type typically causes genital herpes but may also lead to cold sores.
Common symptoms include:
Blisters on the mouth, lips, face, or any area that has come into contact with the infected site.
Itching or tingling sensations in the affected area before blisters appear.
Blisters that may become ulcerated (open sores) and ooze fluid.
Crusting over of the sores within a week of the outbreak.
Swollen lymph glands, which help the body fight infection and inflammation.
Headaches, body aches, and fever.
Like all STDs, the best way to prevent genital herpes is to use condoms and practice safe sex.
Since it is a viral infection, antiviral medications can help speed up recovery. However, these treatments only push the virus into remission; they do not eliminate it completely. Recurrences are possible, especially when the immune system is weakened.
No, there is currently no cure for genital herpes. However, antiviral medications can manage symptoms and reduce the likelihood of transmission.
The frequency of outbreaks varies significantly from person to person. Some individuals may have frequent outbreaks while others may have them rarely or not at all.
Genital herpes does not affect fertility, but it might pose risks during pregnancy. It’s advisable to consult with a healthcare provider if you have genital herpes and are pregnant.
Yes, with proper management and communication with your partner(s), many individuals with genital herpes lead healthy sexual lives.
Using condoms, taking antiviral medications, and avoiding sexual contact during outbreaks can significantly reduce the risk of transmission.
Common triggers include stress, illness, fatigue, sun exposure, and hormonal changes, though triggers can vary between individuals.
Rarely, genital herpes can lead to meningitis or cause rectal inflammation. Also, it increases the risk of HIV transmission.
Yes, it’s possible to be infected with both HSV-1 and HSV-2.
Yes, it’s crucial to communicate with your partner(s) about your STD status to make informed decisions and take necessary precautions.
If you suspect you have genital herpes, you should see a healthcare provider for testing and appropriate management.

Syphilis is a bacterial STD. The first sign of syphilis is a small, painless sore that can appear on the genitals, rectum, or inside the mouth. This sore is called a chancre.
Syphilis is spread only through direct contact with syphilitic chancres. It cannot be transmitted by sharing a toilet, wearing someone else’s clothing, or using another person’s eating utensils.
If left untreated, syphilis can cause serious damage to important organs such as the heart and brain.
During the second stage of syphilis, skin rashes and a sore throat may develop. The rash is typically non-itchy and often appears on the palms and soles, though it may occur anywhere on the body. Some people may not notice the rash before it disappears.
Other symptoms of secondary syphilis may include headaches, swollen lymph nodes, fatigue, fever, weight loss, hair loss, and aching joints.
The final stage of the infection is tertiary syphilis, which can occur years or even decades after the initial infection. Tertiary syphilis can be life-threatening.
Like all STDs, the best way to prevent syphilis is to use condoms and practice safe sex.
Since syphilis is a bacterial infection, it is easily treatable in its early stages with antibiotics.
Syphilis can reoccur if a person is re-exposed to the bacteria, but the previously treated infection does not recur on its own.
Syphilis is diagnosed through blood tests, and in some cases, examination of a sore under a microscope may also be performed.
Syphilis is most contagious in its primary and secondary stages, and during early latent stage. It’s less likely to be transmitted during the late latent or tertiary stages.
Untreated syphilis can lead to severe complications affecting the heart, brain, and other organs, potentially causing life-threatening issues.
While rare, syphilis can be spread through close, non-sexual contact if an uninfected person comes into contact with a syphilitic chancre on an infected individual.
There is currently no vaccine to prevent syphilis. The most effective prevention measures are practicing safe sex and regular testing.
If you suspect you have been exposed to syphilis, it’s important to seek medical attention as soon as possible for testing and potential treatment.
Treatment can help prevent further damage but may not reverse damage already done. It’s crucial to catch and treat syphilis early to avoid reaching this stage.
Yes, syphilis can be transmitted from a pregnant woman to her fetus, which can lead to congenital syphilis, causing severe health issues or stillbirth.
If treated early, there are usually no long-term effects. However, delayed treatment can lead to permanent damage to the heart, brain, and other organs.
Pubic lice, also known as crabs, are tiny insects that live in pubic hair — the hair below the belly button and around the genitals. Pubic lice rarely infest the scalp but can be found in other hairy areas of the body, including the armpits, beard and mustache, chest, eyebrows, and eyelashes.
You get pubic lice through close physical contact with someone who has them. The lice move from the pubic hair of one person to another. Most commonly, people catch crabs through sexual contact. However, even without penetration or intercourse, close physical contact can still lead to transmission.
Occasionally, you can also get crabs through other means — such as by sharing clothing, linens, or towels with an infested person. However, you won’t get crabs through casual contact like handshakes or hugs.
Pubic lice are parasites and can be effectively treated with targeted medications, usually in the form of shampoos and creams.
Yes, while they prefer pubic hair, they can infest other coarse body hair like armpit, chest, or facial hair. However, they rarely infest the scalp hair.
Infestations can spread quickly through sexual contact or close personal contact. It’s important to get treated promptly to prevent spreading the lice to others.
Yes, pubic lice can be seen with the naked eye. They are small, but their presence is often identifiable through their crab-like appearance or the visible eggs (nits) they lay on hair shafts.
Over-the-counter treatments can be effective if used correctly. However, it’s advisable to follow a healthcare provider’s instructions to ensure effective treatment.
Shaving can remove some of the lice, but not the eggs. It’s advisable to use a medication specifically designed to treat pubic lice.
Yes, pubic lice can transfer to bedding, clothing, and towels, although the risk is low. Washing items in hot water and drying them on a high heat setting can kill the lice and their eggs.
After effective treatment, adult lice should die within 24 hours. Follow-up treatment may be necessary to ensure that all lice and eggs are eradicated.
Severe infestations can cause skin irritation, and excessive scratching can lead to secondary bacterial infections. It’s advisable to treat the infestation promptly to avoid complications.
It’s preferable to use a treatment specifically formulated for pubic lice. Consult a healthcare provider for the most effective treatment.
Yes, if you have pubic lice, it’s likely that your sexual partner(s) may also be infested. It’s advisable for all recent sexual partners to be treated at the same time to prevent re-infestation.


MD, DNB - Dermatology & Venereology
Dr. Sejal has dual degrees of MD and DNB in Dermatology and Venereology. She has worked with some of the senior most doctors in the largest government and private hospitals for more than 15 years. Over these years at InUrSKn, she has treated thousands of patients for a variety of conditions and needs across dermatology, venereology, cosmetology and trichology domains.
Dr. Sejal believes in a minimum intervention approach to health and believes that educating and empowering the patient is the key to good health.
Every patient at InUrSkn is seen personally by Dr. Sejal without any time limit, where she discusses the patient’s concern in detail along with understanding the history of their health and carrying out a personal examination.

At InUrSkn, we believe that all patient care must be:
– Holistic
– Personalized
– Humane
– Minimal
Dr. Sejal and her team live by the philosophy of never prescribing medications or procedures that may not be required. When addressing a concern, Dr. Sejal ensures that a detailed history and context are thoroughly understood. Medical tests are prescribed by Dr. Sejal only when she believes there is more to the concern that needs to be addressed, ensuring the patient truly benefits.
Our modern clinic is conveniently located in Powai, Mumbai, and is easily accessible from Hiranandani Gardens, Chandivali, and Vikhroli. Situated close to Dr. L H Hiranandani Hospital, the clinic is also easily reachable from Andheri East, Ghatkopar, and Kanjurmarg via the Jogeshwari–Vikhroli Link Road (JVLR) and the Andheri–Ghatkopar Link Road.
Multiple spacious procedure rooms
Full-fledged operation theatre
In-house laboratory
Latest technology
100+ Skin, Hair & Body Procedures offered
Frequent disinfection of all clinic spaces with UVC light and WHO-approved chemicals
Large waiting and treatment areas to ensure social distancing
Regular health checks for all patients and staff
Safer than salons, chain-clinics & hospitals
PPEs for patients and staff
Personal attention from Dr. Sejal Saheta (MD, DNB) - with 15+ years of experience
CIDESCO-certified aestheticians with minimum 3 years work experience
500+ Positive Reviews on Practo and Google
5000+ Patients treated last year alone
8000+ Procedures completed
| Prices | ||
|---|---|---|
| Procedure | ||
| In Clinic Consultation with Dr. Sejal | ||
| In Clinic Consultation with Dr. Sejal | ₹1200 | |
| Online Consultation with Dr. Sejal | ||
| Online Consultation with Dr. Sejal | ₹1000 | |
Pricing (Inclusive of taxes)


Venereal infections, also known as Sexually Transmitted Infections (STIs) or Diseases (STDs), are infections transmitted through sexual contact.
Practicing safe sex, using condoms, having regular check-ups, and getting vaccinated against certain infections like HPV can reduce the risk.
Many venereal infections are curable with proper medical treatment, but some like HIV are not curable and can only be managed.
Yes, untreated venereal infections can lead to severe health issues including infertility, organ damage, cancer, and increased risk of HIV.
Yes, individuals with multiple sexual partners, those not practicing safe sex, or with a history of STIs are at higher risk.
Yes, many venereal infections can be asymptomatic initially, making regular testing crucial for detection and prevention of transmission.
The frequency of testing depends on individual risk factors. It’s advisable to discuss with a healthcare provider to determine a suitable testing schedule.
Yes, infections like Chlamydia and Gonorrhea, if untreated, can lead to infertility in both men and women.
Yes, being treated for or recovering from a venereal infection doesn’t provide immunity against future infections.
Some venereal infections can be transmitted through non-sexual means such as sharing needles or from mother to child during childbirth.
Common symptoms may include itching, burning, discharge, soreness, rash, or unusual bumps or sores in the genital area.
Oral medications can cure many bacterial venereal infections, but viral infections may require other forms of management. Consultation with a healthcare provider is essential.
Dealing with a venereal infection can lead to stress, anxiety, or depression. It’s important to seek support and counseling if needed.
Yes, some venereal infections can be transmitted from mother to baby during childbirth, which can lead to serious health issues for the baby.
Vaccines are available for some venereal infections like HPV and Hepatitis B. It’s advisable to discuss vaccination options with a healthcare provider.


Ready to book an appointment?
BOOK

Want to talk about your needs ?
MAKE AN enquiry
